Familial Adenomatous Polyposis (FAP)
What is FAP?
This information is intended for anyone affected with FAP, either directly or indirectly. Please share it with your family and with anyone who wants to learn more about this rare precancerous genetic disease. Although FAP may affect only 1 in 10,000 people, it is considered a model for cancer prevention throughout the world. The key to treatment for FAP is education, that is, learning about early diagnosis and appropriate follow-up. The goal of this guide is to help you improve your quality of life by taking an active role in your own health care and that of your family.
Familial means that it runs in families. Each child of an affected parent has a 50 per cent risk of inheriting the disease gene.
Adenomatous is a type of mushroom-shaped growth or polyp which may be precancerous.
Polyposis is a condition where 100 or more polyps can form in the large intestine.
The word "polyp" refers to a lump of cells which form a tissue mass. A polyp must be checked under the microscope (biopsied) to determine whether it is harmless (benign) or precancerous (premalignant). In FAP, abnormal cells form over time and clump together into precancerous adenomas.
Adenomas may be as small as 1-2 mm when they form or as large as 4-5 cm when they change to cancer. Adenomas develop on the surface lining of the intestine, particularly the large intestine.
Where do adenomas grow?
FAP is a disease of the gastrointestinal tract which refers to the stomach, small intestine, and, most particularly, the large intestine.
Digestive Tract
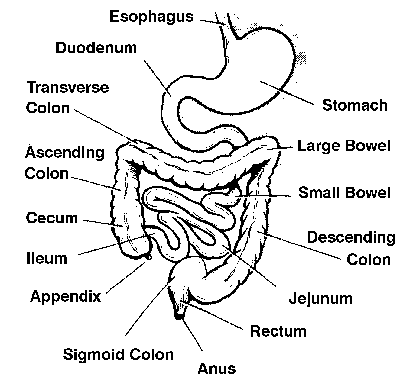
Food passes through the gullet, or esophagus, into the stomach. The stomach is divided into two parts, the opening and the body, or fundus. Digestion takes place in the small intestine which consists of three portions: duodenum, jejunum, and ileum. The duodenum, the shortest part, is an area where adenomas may cluster, especially around the narrow entrance of the bile duct and the pancreas referred to as the ampulla.
The large intestine, divided into the colon and rectum, is approximately 1.5 metres long. Its function is to convert water and minerals, or liquid waste, into a more solid form. It is a warehouse for stool before evacuation takes place through the external opening, or anus. This organ is not required for digestion which occurs in the stomach and small intestine. The large intestine may also be referred to as the large bowel.
Large intestine and portion of small intestine
When do adenomas develop?
Some, not all, people with FAP or attenuated FAP may develop adenomas in the first part of the small intestine, or duodenum.
Duodenal adenomas may appear after the colon is removed and tend to grow much more slowly than colorectal adenomas. Examination is recommended from the age of 25.
The specially designed fibre optic tube is called a side-viewing endoscope which is passed down the mouth and into the stomach and duodenum to carefully inspect the lining of the duodenum and the opening, or ampulla, an area where adenomas may cluster. The forward-viewing endoscope, used in the stomach, is unable to get a clear view of the ampulla which is difficult to see and is often referred to as a blind spot.
In the stomach, two types of polyps may be found in people with FAP or attenuated FAP. The first type is very common and is generally located in the body, or fundus, of the stomach. When biopsied, the result is often a diagnosis of benign fundic gland polyps rather than premalignant polyps. No treatment is necessary and examination is repeated every 5 years. The second type, an adenoma, is uncommon and generally isolated. Treatment depends on the degree of change and size of the adenoma. Examination may be performed every 1 to 2 years.
In the duodenum, most patients will never develop symptoms from adenomas. Depending on the biopsy and appearance of the duodenum, side-viewing endoscopy is repeated at different intervals, ranging from 6 months to 3 years. Treatment may include resection through the endoscope, laser, surgery, or ongoing observation and biopsy.
Since duodenal adenomas are generally slow-growing and may, in fact, be rather small in size and number, an operation is generally not required. New research into medications which can control the growth of duodenal adenomas is underway. As well, genetic information may provide a clue to some families where the risk of developing more extensive duodenal adenomas or duodenal cancer is higher while others have the same low risk as in the general population.
In the jejunum, adenomas are uncommon and difficult to diagnose because this area is hard to see directly. The jejunum may be partially examined by endoscope, or more extensively by x-ray or capsule endoscopy (miniaturized camera in a swallowed pill). Capsule endoscopy provides detailed pictures of the small intestine and passes from the body without harm.
How will I know if I have FAP?
Common symptoms are:
These symptoms are a warning sign indicating the need for bowel examination. Unfortunately, by the time such symptoms occur, a cancer may already have been diagnosed. This may happen when there is just one affected person in the family. Most adolescents in an affected family have NO symptoms at all, only their awareness of the family history of FAP.
Today, we know that symptoms can occur outside the bowel and these may develop years before the formation of any adenomas. An affected parent may have associated symptoms while an affected son or daughter may not. The following description is intended only as a reference.
In 1983, researchers found the earliest known sign of FAP: tiny eye freckles at the back of the retina. These eye freckles occur in up to 85 per cent of people with FAP and may be observed in infants. However, one cannot rule out the risk for FAP or the need for bowel screening if no freckles are found. Freckles cannot be seen without having an eye specialist (ophthalmologist) dilate the pupils and carefully examine the retina. Eye freckles are benign, much like a freckle on the skin.

Eye Freckle
Some people with FAP have a tendency to produce extra tissue in the form of a harmless skin cyst on the scalp, face, arms, or legs. Such cysts are extremely rare in childhood and are strongly associated with FAP. Skin cysts may recur and can be removed, only if necessary, by a specialist to minimize scarring.
Extra tissue may appear as a harmless bony growth in the jaw and, occasionally, a dentist may detect bony growths on a panorex x-ray which gives an all-around view of the upper and lower jaw. Extra sets of tiny, incompletely formed teeth may be another feature. Bony growths may also form on the skull. This may provide another clue to FAP and the need for bowel investigation.
About 10 per cent of people with FAP may develop abnormal bands of tissue called a DESMOID, a benign lesion, most commonly within the wall or lining of the abdomen, and less commonly in the thigh, shoulder, or spine. Due to their complex nature, treatment for a desmoid requires careful evaluation for the appropriate medical or surgical care. In general, surgery is not recommended for desmoids within the lining of the abdomen. The most common method of measuring even slight variations in a desmoid is by a sophisticated x-ray called computerized axial tomography, or CAT-scan, which shows the size and shape of the desmoid, layer by layer.
How is FAP Diagnosed?
Examination of the lower bowel requires the use of a fibre optic tube called a flexible sigmoidoscope which passes through the rectum into the lower bowel, or sigmoid colon, approximately 60 cm. It has a light source, magnifying eyepiece, and open channel through which air may be passed to expand the colon for easier viewing and biopsy.
Flexible Sigmoidoscope
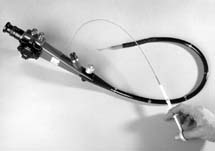
This test is sufficient to diagnose FAP and is initiated from the age of 10 for at-risk children of an affected parent.
Flexible sigmoidoscopy may be done in the doctor's office after a 24-hour bowel preparation. Sedation is not required. Flexible sigmoidoscopy is repeated every two years until age 40 and every 3-5 years until age 60 for each child and sibling of a person with FAP.
A more extensive view of the entire large bowel is provided with a longer tube called a colonoscope. Detailed exploration of problem areas in the large intestine may be carried out. Polyps may be biopsied or removed through the colonoscope. Light sedation is required, along with a specific bowel preparation.
Colonoscopy is suggested as a screening procedure for families with atypical or attenuated FAP since adenomas may predominate in the upper part of the colon. Although the starting age of colonoscopy may be closer to mid- or late-teens for attenuated FAP, the importance of maintaining follow-up care over the years is emphasized. Unlike classical FAP, the likelihood of developing adenomas in attenuated FAP may increase, not decrease, after age 40.
A new test called Virtual Colonoscopy uses a CAT-scan to create a three-dimensional view of the colon. Unlike traditional colonoscopy, no sedation is involved. However, the same bowel preparation is required. Traditional colonoscopy will be needed to biopsy or remove any polyps identified.
Colonoscope

An x-ray of the colon and rectum is not recommended to diagnose FAP because adenomas are often very small and are easily missed or mistaken for stool particles. Moreover, if polyps are observed, the patient will have to return for a scope and biopsy to confirm the type of polyp and degree of change within the polyp.
What is the treatment for FAP?
There is no known medical cure for FAP. Surgery is required because of the large number of adenomas and the 100 per cent risk of colon cancer. In FAP, removal of the large bowel, or colon, is standard treatment and is called colectomy. Since the colon is not primarily involved in how food is digested, you will continue to absorb food in the small intestine.
It is more difficult to accept the need for colectomy when you may feel well. You may ask why surgery cannot be delayed. By the time symptoms do appear, the type of operation and your future may be compromised by the presence of a cancer. Consider the ongoing need for colonoscopy and the possibility of overlooking faster-growing adenomas which have reached the 5-10 year stage. For anyone with FAP, accepting the idea of preventive surgery is the first step.
Through the Familial Gastrointestinal Cancer Registry you can talk with other people with FAP who have had the same operation and get support through a 'buddy system'. Ask for a referral to a colorectal surgeon who specializes in diseases of the large intestine. Bring a list of written questions, or have someone accompany you to the surgeon, so that you will have a better understanding of your treatment.
Timing is an important concern. For school-age patients, the summer months or other holiday time periods during the year are generally preferred. Home tutoring is an option offered by many school boards when surgery occurs during the school year. Talking with the guidance counsellor and home room teacher will enable parents to plan accordingly. It is important to include adolescents in these plans and to prepare them for their hospital stay. Remember that most patients with FAP are asymptomatic and otherwise well, improving their healing ability and recovery. We provide children's books, instructional videos and relaxation tapes to help with the emotional and physical preparations for the procedure.
The following operations all include removal of the colon (colectomy) and focus on the rectum. The stage of disease and the number of adenomas in the rectum may influence the type of operation which is recommended for each person with FAP. Ask your surgeon whether your surgery can be done laparoscopically (through the abdomen) to reduce scarring. It involves the used of special telescopies, cameras and instruments designed to fit through small operating tubes.
Ileorectal Anastomosis, or IRA, means that the last part of the small intestine (ileum) is joined (anastomosed) to 10-15 cm of the rectum. This procedure may be suggested for someone who has minimal rectal adenomas. The average hospital stay is 7 days. The average recovery time at home is 6 weeks.
Since you will experience several bowel movements a day, it may be helpful to talk with a dietitian about your own diet. Some people report no food intolerances while others discover that a food diary may be helpful post-operatively In general, remember that potential problem foods may only be a concern as the body adapts and this may take up to a year. You will be your own best food detective and should not restrict yourself unnecessarily. Anyone who has an IRA retains part of the rectum which must be checked every 6 months to l year for life. As long as the lining of the rectum remains intact, adenomas may form. A hollow metal instrument with a light source, called a Sigmoidoscope, is generally used and no sedation is required. Bowel preparation is needed to clear the rectum of stool and gas.
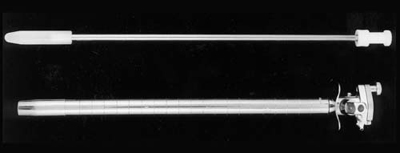
Sigmoidoscope
Restorative proctocolectomy, also known as the pelvic pouch, is generally a two-stage procedure. In the first operation, after colectomy, the upper part of the rectum and lining of the lower rectum are removed. The muscles controlling the urge for a bowel movement remain. A new rectum is created from the patient's own ileum in the form of a pouch which is brought down into the pelvis and joined to the anus.
Time is needed for the area to properly heal and to ensure good function of the pouch. For this reason, a temporary opening (stoma) is made from the ileum to the outside of the abdomen. An external appliance is worn to collect waste products and is referred to as an ileostomy. During the average 10-day hospital stay, a specialist nurse called an enterostomal therapist, or ET, will teach you how to manage your ileostomy. Prior to your admission, you will have a chance to meet the ET and to ask questions so that you are better prepared for your operation. The dietitian will discuss the need to maintain a diet during this healing period and to ensure an adequate intake of fluids. You can ask for an illustrated pelvic pouch booklet to guide you with detailed explanations. A support group for people with a pelvic pouch is available at Mount Sinai Hospital. An x-ray of the pouch is taken after 6 weeks to ensure that the pouch is functioning. In general, the second operation is performed after 3 months and is a brief procedure to close the ileostomy, followed by an average 6-day hospital stay. The number of bowel movements varies in individuals but adjustments in diet or medication may be needed, either during the recovery period or long term.
Anyone with a pelvic pouch will require regular examination of the pouch to rule out any new adenomas. This operation may be recommended for anyone with a large number of adenomas in the rectum. Due to the technically demanding nature of the procedure, pelvic pouch surgery should be performed by experienced surgeons.
Proctocolectomy means that the entire colon and rectum are removed. A permanent ileostomy is formed and a stoma is created, usually to the right and below the navel so that waste products can pass into an external appliance. This operation is not a common option for FAP but may be suggested if rectal cancer is found; or a desmoid tumour has formed within the abdomen; or other technical problems such as scarring are identified in the ileum. The average hospital stay is 10 days. In the pre- and postoperative period, the ET nurse will not only teach you how to manage your ostomy but will offer practical suggestions. The presence of an ileostomy does not prevent sexual relations. There is a period of adjustment for both partners who may benefit by sharing their concerns with each other, the patient's doctor, and the ET nurse. During the recovery period, this support may strengthen how a patient feels about himself or herself as a person. Sexual expression is a total body response involving emotional and physical needs which allow us to reach out to others. The United Ostomy Association of Canada, provides assistance through local chapters, trained visitors, and the "Ostomy Canada" journal.
Women with an ileostomy may conceive. To allow for adequate healing, patients are encouraged to wait at least 1 year after bowel surgery before becoming pregnant. X-rays of the colon should be postponed until after the child is born, although other diagnostic procedures may be carried out during pregnancy.
Continent ileostomy, or Kock pouch, involves the removal of the colon, rectum, and anus. An internal abdominal pouch is created with a nipple-shaped valve to prevent stool from leaking. The end of the ileum is brought to the surface of the abdomen and a stoma is fashioned. To empty waste products, you insert a tube into the pouch. A gauze patch is worn over the stoma. No external appliance is needed. This operation is performed infrequently today and 10-20 per cent of people with a Kock pouch have required surgical revision of the nipple valve due to its intricate nature.
Where else can Adenomas Develop?
Some, not all, people with FAP or attenuated FAP may develop adenomas in the first part of the small intestine, or duodenum.
Duodenal adenomas may appear after the colon is removed and tend to grow much more slowly than colorectal adenomas. Examination is recommended from the age of 25.
The specially designed fibre optic tube is called a side-viewing endoscope which is passed down the mouth and into the stomach and duodenum to carefully inspect the lining of the duodenum and the opening, or ampulla, an area where adenomas may cluster. The forward-viewing endoscope, used in the stomach, is unable to get a clear view of the ampulla which is difficult to see and is often referred to as a blind spot.
In the stomach, two types of polyps may be found in people with FAP or attenuated FAP. The first type is very common and is generally located in the body, or fundus, of the stomach. When biopsied, the result is often a diagnosis of benign fundic gland polyps rather than premalignant polyps. No treatment is necessary and examination is repeated every 5 years. The second type, an adenoma, is uncommon and generally isolated. Treatment depends on the degree of change and size of the adenoma. Examination may be performed every 1 to 2 years.
In the duodenum, most patients will never develop symptoms from adenomas. Depending on the biopsy and appearance of the duodenum, side-viewing endoscopy is repeated at different intervals, ranging from 6 months to 3 years. Treatment may include resection through the endoscope, laser, surgery, or ongoing observation and biopsy.
Since duodenal adenomas are generally slow-growing and may, in fact, be rather small in size and number, an operation is generally not required. New research into medications which can control the growth of duodenal adenomas is underway. As well, genetic information may provide a clue to some families where the risk of developing more extensive duodenal adenomas or duodenal cancer is higher while others have the same low risk as in the general population.
In the jejunum, adenomas are uncommon and difficult to diagnose because this area is hard to see directly. The jejunum may be partially examined by endoscope, or more extensively by x-ray or capsule endoscopy (miniaturized camera in a swallowed pill). Capsule endoscopy provides detailed pictures of the small intestine and passes from the body without harm.
Who is at Risk for FAP?
Each child of a parent with FAP or attenuated FAP has a 50 per cent risk of inheriting the disease gene. If an affected parent has four children, this does not mean that two children will have FAP. The chances are the same in each pregnancy that the FAP gene will be passed on by the parent with FAP. FAP affects males and females of every race and ethnic group. FAP does not skip generations.
In the past, neither doctors nor scientists could predict who would be diagnosed with FAP until adenomas developed in the large intestine. However, in 1991, the gene responsible for FAP was discovered and was named the Adenomatous Polyposis Coli, or APC, gene.
Genes are the units of heredity which decide our sex, eye/hair colour, build, and, sometimes, susceptibility for certain diseases. We now know that about 100,000 genes do their work inside each human cell. Genes contain all the information the cell needs to carry on its production of protein and energy, like an encyclopedia.
Deoxyribonucleic acid, or DNA, is the language of the genes, the master chemical. When cells divide, the genes and DNA copy themselves. Genes are found in separate strands of DNA called chromosomes. We inherit 23 pairs of chromosomes and one member of each pair comes from each parent.
When copying takes place perfectly, genetic information is passed from one generation to the next. However, if even a tiny change occurs, either the structure or the functions in the body may be dramatically different. For example, the word "milk" makes perfect sense until one letter is switched: "xilk". This change is called a mutation. If left unrepaired, the change is passed on and can contribute to a particular disease.

Diagram of DNA, a molecule carrying genetic information
(Reproduced with permission by Jeanne C. Kelly, Aardvark Design Associates.
Original artwork for the National Cancer Institute, Bethesda, Maryland.)
Where can I Learn More about FAP?
One way of understanding who is, and who is not, at risk for FAP is by starting a family tree and keeping it up to date.
The Familial Gastrointestinal Cancer Registry, at Mount Sinai Hospital in Toronto, was established in 1980 to assist Canadian patients with FAP and their families. The first step is to draw the family history so that each child, brother, and sister of someone with FAP can become aware of their risk and what they can do to prevent bowel cancer. We welcome help from family members in updating us when someone moves, marries, or has a child. We also ask patients to let us know the results of their check-up each time they see their doctor or undergo surgery.
Part of our service involves referral on request to specialists with a particular interest in FAP. When travelling, it is useful to know the nearest specialty centre where medical care is available. Families are encouraged to add to their knowledge of FAP by reading related articles or pamphlets from our patient library, looking at videos, and listening to audio tapes.
If you would like to know more about FAP, please contact us
